The majority of conversations surrounding blood sugar issues like diabetes, hypoglycemia, and insulin resistance are focused on macronutrients. The immediate reaction is to ask about the dietary balance of carbs, proteins, and fats, which can be partially misguided. Balanced meals are an essential part of blood sugar balance and a crucial component of adrenal and thyroid health. However, if someone is dealing with many spikes and dips in their blood glucose, we have to fight the temptation always to assume that their macronutrient ratio is off due to carbohydrate consumption. Yes, eating carbs does cause your blood sugar to rise, and depending on the person, it may lead to a severe drop. For this reason, low-carb diets have exploded in popularity over the last decade, slowly phasing out the fear of fat ignited by physiologist Ancel Keys in the 1950s and replacing it with a deep-seated disdain for anything that turns to glucose in the blood.
These days society pushes a different diet on us for every symptom. Overweight? Try the Atkins Diet. Have blood sugar issues? Follow the Keto Diet. Are you feeling sluggish? The Carnivore Diet will change your life. The current consensus is that we simply don’t need carbs to survive. We’re starting to see with our clients that the demonization of this particular macronutrient is leading to disordered eating tendencies in women and a worsening of symptoms overall. Which leads us to ask the question: Is the consumption of carbs over time the culprit of metabolic issues like PCOS and insulin resistance? Or is there something else at play here? To get to the bottom of this problem, we have to look at all of the information we have available to us about what impacts blood sugar regulation—and minerals is a big one. Let’s get specific.
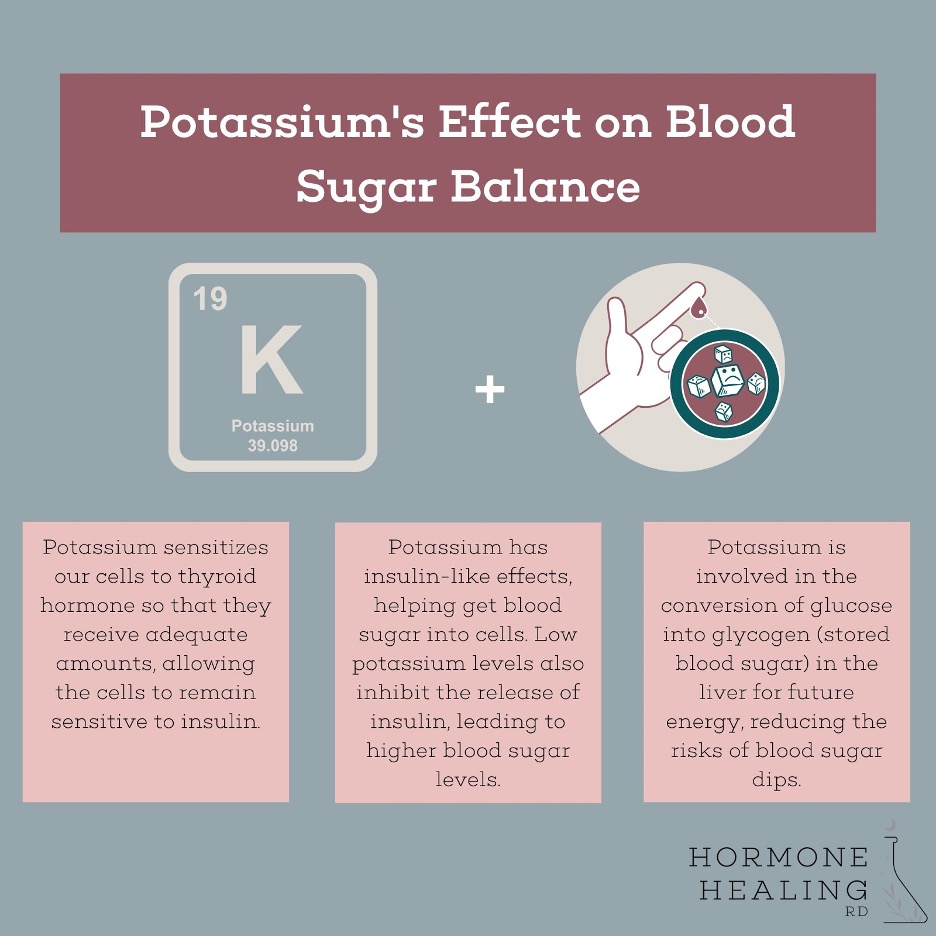
Potassium’s Effect On Blood Sugar
We’ve discussed the importance of potassium for so many different functions in the body (including regulating blood pressure, maintaining fluid balance and pH of the body, impacting nerve conduction in the heart, and dilating arteries) but how exactly does it support blood sugar balance?
The answer is three-fold:
This may be why we’re seeing recent research suggest that lower levels of potassium in the blood can lead to greater risk of developing Type 2 Diabetes. And interestingly, the best way to get potassium through your diet is with carbs, especially potatoes, coconut water, squash, and fruit.
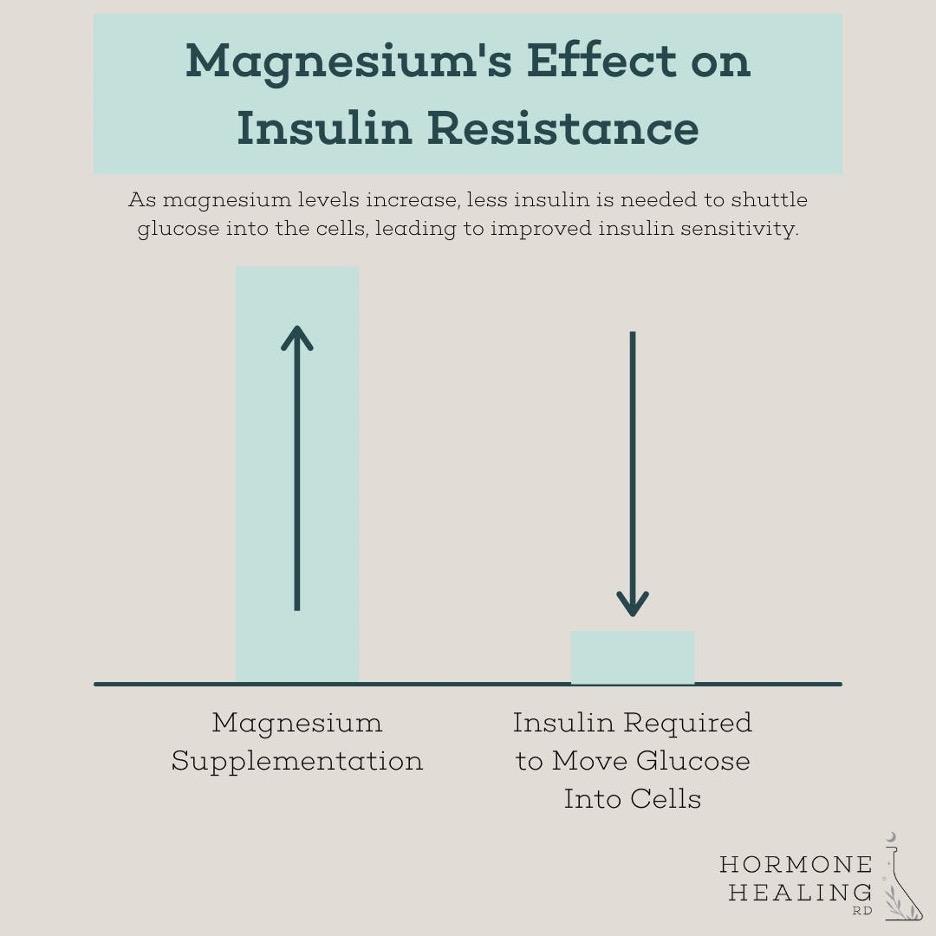
Effects of Magnesium on Blood Sugar
Women’s Health Naturopath, Lara Briden, calls magnesium the “natural Metformin” because of its ability to regulate blood sugar and normalize insulin. So, what does magnesium do to support blood sugar balance?
Hyperinsulinism causes low blood sugar in the short term, but in the long run, the pancreas will wear itself out, and the cells in the body will become resistant to insulin, resulting in—you guessed it—high blood sugar levels. Overall, chronically low magnesium levels can impair the action of insulin and increase insulin resistance, contributing to conditions like PCOS and Type 2 Diabetes.
Effects of Calcium on Blood Sugar
The role that calcium plays in blood sugar balance is slightly different from that of potassium and magnesium. While calcium does have its own set of functions and health benefits, an overabundance of calcium in the body can have a negative effect on blood glucose levels. Why is that? High calcium levels often show up as a result of chronic stress and can lead to a deficiency or loss of magnesium, sodium, and potassium. When these mineral ratios are out of whack in calcium’s favor, many problems can arise in the body. Here are different ratios and what they mean:
For lowering calcium, a vitamin K supplement helps usher this mineral out of soft tissue cells and putting it in places where it should be, like bones and teeth. Iodine therapy can also help with elevated calcium, but we don’t recommend doing this without the supervision of a health professional.
Not sure if your minerals are out of whack? Take our mineral quiz to find out whether or not yours might need support!
And if you want to learn more about minerals and how they impact your hormones in general, check out this free training we hosted recently on optimizing your hormone health with mineral balance. We walk you through mineral foundations and three steps to addressing mineral imbalances, including how to test your own. PLUS, you’ll get a free copy of our Mineral Imbalance Cheat Sheet, which breaks down common mineral imbalances and symptoms that typically accompany them.
When treating conditions like PCOS, insulin resistance, and diabetes, we can’t just look at macronutrients. There is so much more to the blood sugar puzzle, and I’d say that micronutrients are a BIG factor in glucose metabolism and regulation. Despite what mainstream health experts will have you believe, the answer is not always to eliminate or minimize carbohydrates in the diet. Doing so is only placing a temporary band-aid on a much deeper issue. It’s only when we balance our minerals like calcium, sodium, potassium, and magnesium that we’ll begin to see actual progress in blood sugar balance.
